September 17, 2024
2 min read
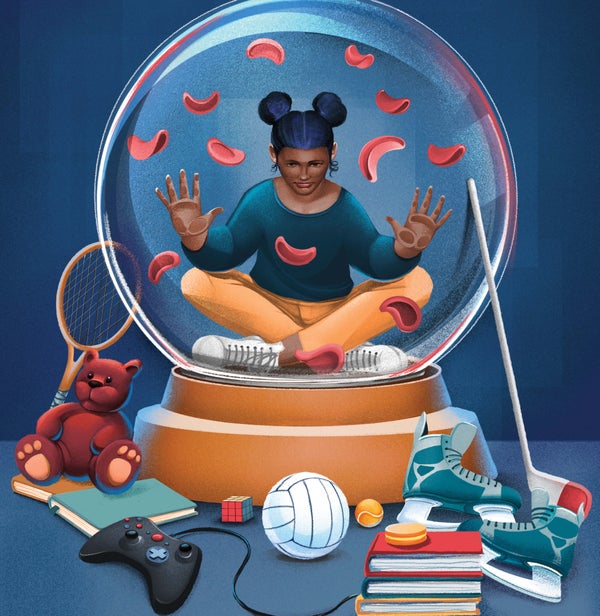
New Hope for Treating People with Sickle Cell Disease
Improving sickle cell care by expanding treatment options, advancing new therapies and amplifying the voices of people with the disease
This article is part of “Innovations In: Sickle Cell Disease,” an editorially independent special report that was produced with financial support from Vertex Pharmaceuticals.
The oldest known evidence of sickle cell disease has been traced back more than 7,000 years, and the illness was first described in medical literature more than a century ago. It was the first molecular disease to be understood, a single mutation in a single gene that causes a heritable illness. When someone has one copy of the mutated gene, the trait is often asymptomatic, but when someone inherits a copy from each parent, the disease can become excruciating. The mutation results in abnormal hemoglobin, which causes red blood cells to curve into a characteristic sickle shape and to become stiff and sticky; ultimately the sickled cells fail to deliver oxygen efficiently to tissues throughout the body. Untreated, the disease can cause sepsis, pneumonia, strokes and heart attacks, and it brings on the punishing pain that occurs when blood vessels are blocked during vaso-occlusive episodes.
The disease affects millions of people across the world—some estimates suggest as many as 20 million—but despite its historical significance and widespread incidence it remains underfunded, understudied and undertreated. Those with the disease in the U.S. benefit from screening and treatment from birth, which over the past 50 years has extended the average patient’s lifespan from 14 to 53 years. But people too often encounter a biased medical system that tends to mistrust their reports of extreme pain and accuse them of drug seeking. In the low-income countries where sickle cell is most prevalent and newborn screening for the disease is limited or nonexistent, too many children with sickle cell do not live past five years old.
On supporting science journalism
If you’re enjoying this article, consider supporting our award-winning journalism by subscribing. By purchasing a subscription you are helping to ensure the future of impactful stories about the discoveries and ideas shaping our world today.
Patients, physicians, researchers and advocates are pushing for change. Some are expanding screening and treatment options in places such as sub-Saharan Africa, as technology has allowed for more accurate, portable options. Others are illuminating patient experience, showing sickle cell pain to be some of the most intense ever experienced and seeking new ways to both prevent it and alleviate suffering once it sets in. They are pursuing increased funding and new public health policies to ease the burden on low-income nations, to improve patients’ lives and to further genomic medicine research. And they are moving new therapeutics through the discovery pipeline and into clinics, where patients are just beginning to reap the benefits. Above all, they are lifting up the voices of people with sickle cell disease, who have been dismissed for far too long.

